Knee anatomy. Knee examination methods
The knee joint is the largest and most often damaged in the human musculoskeletal system due to its structure, high functional requirements for it, and vulnerability to external forces. Knowledge of normal anatomy is the key to diagnosing and treating knee injuries and diseases.
Conventionally, in the knee joint, bone structures, extra-articular and intra-articular soft tissue formations can be distinguished.
Three bone formations are involved in the formation of the knee joint:
condyles of the femur;
tibial condyles;
the patella, which, along with the previous formation, forms the femoral-tibial and femoral-patellar joints.
The condyles of the femur are two rounded eccentrically curved eminences. At the front, they are somewhat flattened, which creates a large area for contact and distribution of loads. Between the condyles in front there is a femoral-patellar groove for articulation with the articular surface of the patella. Posteriorly, the condyles are separated by the intercondylar notch.
The condyles of the tibia form a flat surface, the so-called plateau of the tibia, articulating with the condyles of the femur. In the middle, the condyles of the tibia are separated by the intercondylar eminence, on which the internal and external intercondylar tubercles are located, serving as the place of attachment of the cruciate ligaments and menisci. The posterior edge of the lateral tibial condyle is flattened in the area where the external meniscus slides posteriorly during knee flexion.
The articular surfaces of the femoral-tibial articulation are incongruent and therefore stability is provided only by soft tissue formations.
The patella is a trihedral sesamoid bone, wide at the proximal pole and tapering towards the distal pole. The articular surface of the patella is divided by a vertical ridge into inner and outer articular facets, or surfaces. When extending in the knee joint, the patella is located at the upper edge of the articular surface of the femoral-patellar groove, the distal part of its outer facet articulates with the outer condyle of the femur. Further, as flexion progresses, the zone of maximum contact shifts to the middle of the patella, and then, with full flexion, the proximal parts of both patellar facets contact the femur, with more pressure on the inner facet.
In the knee joint, the anterior, internal and external sections are conventionally distinguished. The inner and outer sections are formed by the articular surfaces of the inner and outer condyles of the femur and tibia, respectively, and the anterior section is formed by the facies articularis of the patella and the patellar groove of the condyles of the femur.
Traumatic effects often disrupt the normal relationship of bone structures, therefore, the key to restoring the function of the knee joint is anatomical reposition of fragments of the articular surfaces.
The articulating condyles of the femur and tibia are incongruent, which allows for significant freedom of movement in the joint. In this case, a stabilizing role belongs to soft tissue structures, which include menisci, capsular-ligamentous apparatus and muscle-tendon complexes.
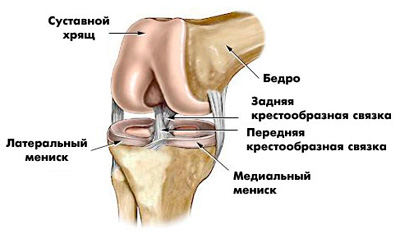
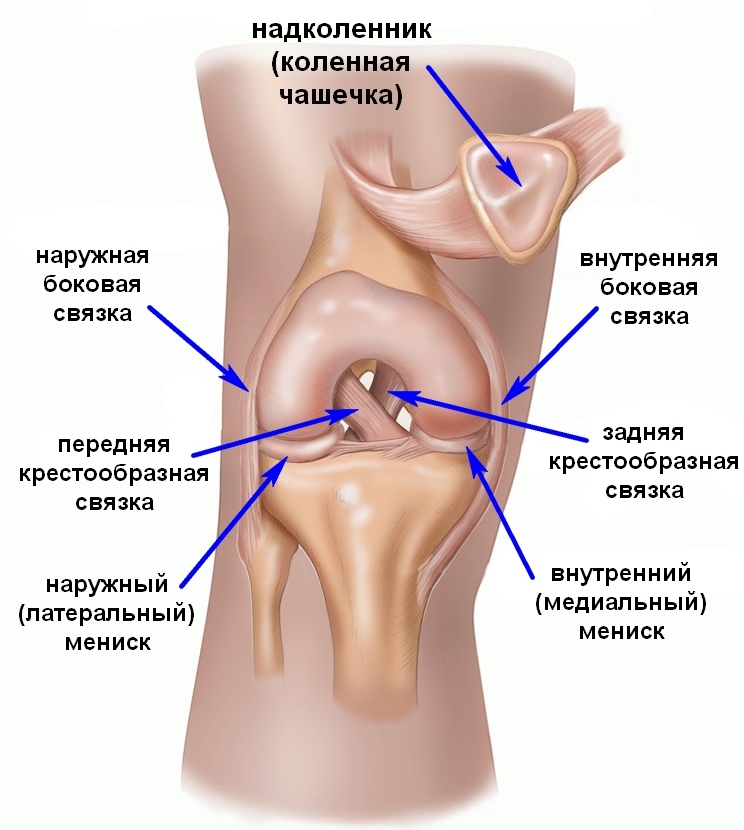
The main intra-articular soft tissue structures are the inner and outer menisci, as well as the anterior and posterior cruciate ligaments.
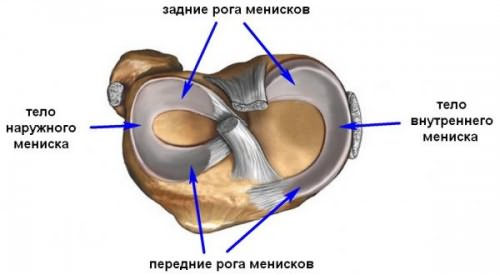
The inner and outer menisci are semilunar formations, approximately triangular in cross-section, covering from one to two thirds of the corresponding part of the tibial plateau. Their lower surface is flat, and the upper one is concave. They are formed by tightly woven collagen fibers, most of which are oriented in a circle, but there are also fibers that run radially and from the bottom up, as we call perforating. This structure of the meniscus provides high elasticity and the ability to resist compression. A significant part of the menisci are avascular, as a result of which their reparative capabilities are limited. In an adult, blood vessels are present only in the peripheral parts, no more than 1/4 of the meniscus width. The menisci are firmly attached to the joint capsule throughout. An exception is the opening in the posterior third of the external meniscus, through which the hamstring muscle passes intra-articularly to the site of its attachment on the external condyle of the femur.
The outer meniscus is smaller in diameter than the inner one, but wider and thicker. Due to attachment to both cruciate ligaments, to the inner condyle of the femur through the anterior menisto-femoral ligament or posterior menisto-femoral ligament and to the popliteal muscle, it is more mobile and damaged less often than the narrow and thin internal meniscus, not associated with the cruciate ligaments and throughout the length is firmly attached to the capsule by means of the coronary ligament. The front horns of the menisci are connected by a transverse ligament. When unbending, the menisci are displaced anteriorly, when flexed posteriorly.
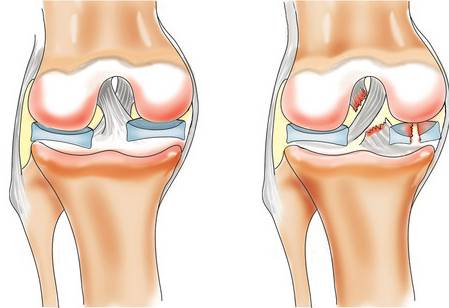
Circular fibers act like metal hoops in a filled wooden barrel - the tension in the hoops holds the boards up. When the menisci are compressed by the condyles of the femur and tibia, forces are generated that push the menisci to the periphery. Circulatory tension in the menisci counteracts these outwardly directed radial forces, and they are tangentially transmitted evenly to the articular cartilage overlying the tibial plateau through the strong anterior and posterior meniscus attachments. When the radial rupture spreads to the capsular zone, the effect of circular stress disappears, which leads to a sharp increase in pressure per unit area and the development of degenerative changes in cartilage and bone tissue.

Thus, menisci perform the following important functions:
First, they compensate for the incongruence of the articular surfaces of the condyles of the tibia and femur and are involved in shock absorption and even distribution of loads on the articular surfaces of the articulating bones. After removing the inner meniscus, the contact area is reduced by 40%.
Secondly, they prevent the capsule and synovium from being pinched during joint movements.
Third, the menisci help the distribution of synovial fluid throughout the joint, thereby contributing to the hydration and nutrition of the cartilage.
Fourthly, they contribute to the stabilization of the joint in all planes, their effect on ensuring rotational stability is especially important.
Other important structures located inside the joint are the anterior and posterior cruciate ligaments, separated by two bundles: the anterior-internal, stretching during flexion, and the posterior-external, carrying the main load during extension. Thus, at any position of the joint, the ACL maintains a constant tension, controlling the relationship between the condyles of the femur and tibia. The ACL limits the anterior displacement of the tibia and its rotation. The PCL is stronger and shorter than the anterior one. It begins in the anterior part of the outer surface of the inner condyle of the femur and, following posteriorly and outwardly, is attached to the posterior surface of the proximal end of the tibia, some of the fibers are woven into the posterior parts of the joint capsule. In it, two beams are also conventionally distinguished: antero-external and posterior-internal. The main function of the ZKS is to prevent posterior displacement, hyperextension of the lower leg and rotation.
The most stable position of the knee joint is full extension. The least stable is flexion within 120-160 °, in which the relaxation of the posterolateral capsule-ligamentous structures is combined with the insufficiently effective action of dynamic stabilizers. In this critical range, the stability of the joint is primarily provided by the ACL, which determines its increased vulnerability.
The most important extra-articular soft tissue educated include:
synovium;
fibrous capsule;
collateral ligaments;
muscle-tendon complexes covering the knee joint, such as the quadriceps femoris, gastrocnemius, biceps femoris, semitendinosus, semimembranous, tender, sartorius, popliteal muscles, and the iliotibial tract.
Extra-articular muscle-tendon formations, which are dynamic stabilizers of the knee joint. On the anterior surface of the knee joint, the four heads of the quadriceps femoris form a common three-layer tendon that attaches to the patella. The anterior layer is made by the tendon of the rectus femoris, starting from the anterior superior iliac spine and attaching to the anterior edge of the superior pole of the patella. The patellar tendon, starting at the intertrochanteric line on the anterior surface of the femur, attaches to the posterior edge of the superior pole of the patella, forming a deep layer. The middle layer is formed by the vastus medialis and vastus lateralis tendons. The patellar ligament runs from the lower pole of the patella to the tuberosity of the tibia. The main function of the quadriceps muscle is to extend the knee joint.
The distal extensions of the aponeurosis of the vastus medialis and vastus lateralis form a tendon stretch that is woven into the joint capsule, retinaculum patellae mediale et laterale. From the inside, it attaches along the medial edge of the patella and patellar ligament and distally to the tibia. Its function is to keep the patella in the femoral-patellar sulcus during movement, or, in other words, to prevent the patella from shifting outward when bending the knee joint. The key formation in this zone is considered to be the compacted cord of the retainer - the internal patellofemoral ligament.
From the outside, a tendon stretch is attached to the outer edge of the patella and to the ilio-femoral tract, helping to tighten the latter during knee extension.
An imbalance between the structures of the medal and lateral retainer always occurs with subluxation and dislocation of the patella.
The gastrocnemius muscle is closely soldered to the posterior surface of the knee joint capsule and its two heads are attached to the posterior surface of the inner and outer condyles of the femur, limiting the popliteal fossa from below. Function - flexion at the knee joint.
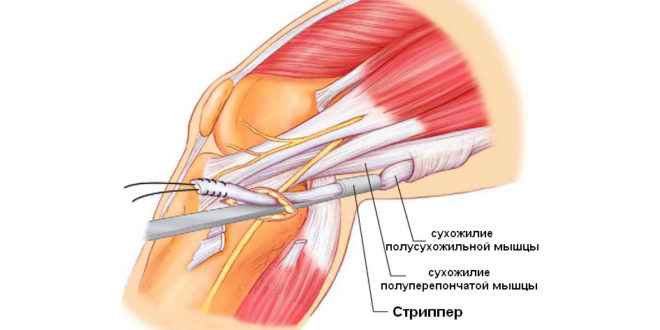
Goose foot is a joint attachment of the tendons of the sartorian, tender and semitendinosus muscles on the inner surface of the proximal tibia. Their primary function is flexion in the knee joint, the secondary function is to rotate the tibia inward and resist rotational and valgus loads. Proximally, the sartorius muscle attaches to the anterior superior iliac spine, the tender muscle to the anterior surface of the pubic bone, and the semitendinosus muscle begins on the ischial tuberosity.
The antagonist of the crow's feet on the outer surface of the knee joint is the attachment of the biceps femoris to the head of the fibula, the outer surface of the tibia, and the posterior outer part of the joint capsule. Its proximally long head originates from the upper inner surface of the ischial tuberosity and the sacro-tuberous ligament, and its short head originates from the lateral lip of the rough line of the femur. This muscle is a powerful flexor and external rotator of the lower leg. It also provides rotational stability, preventing anterior displacement of the lower leg during flexion at the knee joint. The continuation of its tendon fibers is the arcuate popliteal ligament, which, together with other structures of the posterior-outer part of the joint capsule, provides rotational and varus stability.
The popliteal muscle originates from the posterior surface of the tibia and attaches to the outer condyle of the femur, to the head of the fibula, through the so-called popliteal-peroneal ligament, and to the posterior horn of the external meniscus. Continuations of these attachments form the arcuate popliteal ligament - lig. arcuatum, starting from the head of the fibula and woven into the back of the joint capsule. The popliteal muscle is the internal rotator of the tibia at the initial angles of flexion in the knee joint and displaces the external meniscus posteriorly during flexion. In addition, it contributes significantly to maintaining rotational stability and assists the posterior cruciate ligament in preventing anterior displacement of the femur relative to the tibia.
The semimembranous muscle is an important stabilizing structure of the posterior and posterior-internal parts of the knee joint. It begins with a flattened tendon from the ischial tuberosity. There are five main areas of its attachment.
The first is a continuation into the oblique popliteal ligament, which extends from the attachment of the semimembranous muscle to the posterior-inner surface of the tibia obliquely and outward in the direction of attachment of the outer head of the gastrocnemius muscle. The semimembranous muscle, when contracted, stretches the oblique popliteal ligament.
The second tendon attachment is woven into the posterior surface of the fibrous capsule of the joint and the posterior horn of the internal meniscus, ensuring its posterior displacement during flexion in the joint. Anterior or deep head m. semimembranosus runs along the inner surface of the tibia and is attached under the superficial portion of the tibial collateral ligament, slightly distal to the joint space. The straight head of the semi-membranous muscle attaches to the tubercle on the posterior surface of the inner condyle of the tibia, just below the joint space. The distal portion of the semimembranous muscle forms a fibrous cleavage covering the popliteal muscle and then woven into the tibial periosteum. Thus, when reducing m. semimembranosus, tension of all the above formations of the posterior inner surface of the knee joint, including the posterior capsule, occurs, providing stability. Functionally, the semimembranous muscle acts as a flexor and internal rotator of the lower leg.
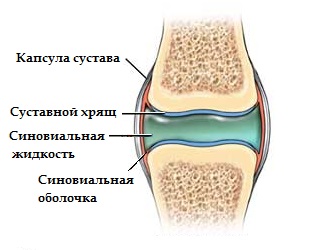
Knee capsule
The knee capsule and collateral ligaments are the main extra-articular static stabilizing structures. The knee capsule is attached to the edges of the articular surfaces of the articulating bones and consists of durable fibrous and synovial layers. The synovium lines the non-cartilaginous surface of the joint. In the knee joint, it forms folds, the most significant of which are suprapatellar, infrapatellar, mediopatellar and lateral. In various pathological conditions, they can increase and thicken, while losing elasticity, which, in turn, leads to limitation of movements in the joint, especially flexion. Sometimes intra-articular bodies are hidden in the thickness of the synovial folds. The most common surgical treatment is the mediopatellar fold.
In addition to folds, the synovial membrane forms twists that increase the volume of the joint cavity. The largest is the patellar synovial bag, located behind the tendon of the quadriceps femoris. The bursae of the popliteal, semimembranous and inner head of the gastrocnemius muscles usually communicate with the joint cavity. There are a number of mucous bags that are not connected to the joint cavity: bursa m. gastrocnemii lateralis, bursa anserina, bursa infrapatellaris, bursa prepatellaris subcutanea, bursa prepatellaris subtendinea, bursa prepatellaris subfascialis, etc.
The main internal extra-articular static stabilizer of the knee joint is the internal, or tibial, collateral ligament. It consists of two portions: superficial and deep. The superficial part contains long fibers and runs from the inner epicondyle of the femur to the metaphysis of the tibia, attaching 5-7 cm below the articular line. The deep part consists of short fibers closely connected with the inner meniscus, and forming the menisto-femoral and menisto-tibial ligaments. The main function of the tibial collateral ligament is to prevent excessive valgus deviation and outward rotation of the lower leg. When flexing at the knee joint, it is displaced posteriorly and when extended anteriorly.
Posterior to the tibial collateral ligament is the posterior medial part of the joint capsule, the main element of which is the posterior oblique ligament, which extends from the adductor tubercle on the inner condyle of the femur obliquely in the posterior caudal direction. Its distal attachment consists of three parts: the most pronounced and most important central one - at the articular edge of the posterior-inner angle of the tibial plateau, near the attachment of the straight head of the semi-membranous muscle. The upper one is woven into the posterior capsule of the joint and the proximal part of the oblique popliteal ligament. The lower, or distal, part of the fibers merges with the aponeurosis of the semimembranous muscle tendon at the site of its attachment.

The posterior-inner part of the joint capsule makes a significant contribution to ensuring the valgus and rotational stability of the knee joint. As the knee is flexed, the tone of the posterior-internal capsule and the posterior oblique ligament progressively decreases, however, with active contraction of the semi-membranous muscle, all three bundles of the posterior oblique ligament are stretched, thus realizing both static and dynamic stabilizing effects, even with a bent knee joint.
The external, or peroneal, collateral ligament is the main stabilizer that counteracts varied loads during extension in the knee joint; as it flexes, its stabilizing significance decreases. Proximally, it attaches to the outer epicondyle of the femur, distally to the head of the fibula. During tractas iliotibialis knee flexion, the hamstring tendon and the peroneal collateral ligament cross each other, while the biceps femoris tendon and the iliotibial tract remain parallel as in extension, which increases the lateral stability of the joint. Attachment of the popliteal muscle to the fibula, femoral condyle and posterior surface of the tibia is extremely important in preventing posterior displacement, varus deflection and outward rotation of the tibia, which must be taken into account when performing reconstructive operations on the lateral capsule-ligamentous complex.
Inner and outer menisci
Blood supply and innervation
The blood supply to the muscles that perform movements in the knee joint is carried out by the femoral artery and its branches: the deep artery of the thigh, the medial and lateral circumflex arteries, perforating arteries, the descending artery, and the popliteal artery. The blood supply to the knee joint is carried out by the branches of the popliteal artery, which form the articular network of the knee region. The popliteal artery, being a continuation of the femoral artery, begins at the level of the lower opening of the adductor canal, passes under the semimembranous muscle, then along the bottom of the popliteal fossa, adjacent to the posterior capsule of the knee joint, and in the lower part of the popliteal fossa - to m. popliteus. Having reached the soleus muscle, the popliteal artery is divided into the anterior tibial and posterior tibial artery. The popliteal artery is accompanied by the vein of the same name and n. tibialis. In its course, the popliteal artery gives off a series of branches that supply blood to the muscles and the knee joint. Widely anastomosed with each other, they form a dense vascular articular network of the knee. Among the branches of the popliteal artery, the upper muscle branches, the lateral and medial upper knee arteries, the middle knee artery, the lateral and medial lower knee arteries extending at the level of the joint space, and the gastrocnemius arteries are distinguished. Thus, the knee joint has an abundant blood supply, which contributes to good tissue regeneration after injuries and surgeries.

The femoral and sciatic nerves are involved in the innervation of the muscles of the thigh and lower leg. The femoral nerve is mixed, contains muscle and sensory branches. The latter accompany the subcutaneous branches of V. saphena magna and form n. saphenus, connecting in the femoral fossa with muscle branches.
The sciatic nerve at the superior corner of the popliteal fossa is divided into the tibial and common peroneal nerves. The latter, bending around the outer head of the gastrocnemius muscle, passes posteriorly and inwardly from the tendon of the biceps femoris muscle, then crossing the neck of the fibula. Due to its superficial location, it is prone to damage more often than other nerve structures in the knee joint.
Biomechanics
The main movements in the knee joint are flexion and extension, in addition to which abduction and adduction are possible, as well as inward and outward rotation when the limb is bent at the knee joint. Due to the fact that the condyles of the femur are eccentric, the transverse axis. around which flexion and extension in the knee joint occurs, is not fixed, but constantly changes its position, describing a curve in the form of a comma - polycentric rotation.
The complex flexion-extension movement is a combination of rolling and sliding between the condyles of the femur and tibia. Rolling occurs at the first 20 ° of flexion, then gradually the movements take on a predominantly sliding character. Rolling in the first 20 ° of flexion better meets the knee stability requirements, while sliding as it flexes gives more freedom for rotation. The configuration of the bone structures and the tone of the ligaments and menisci do not allow for rotational movements with full extension. As flexion progresses, the capsule, lateral and cruciate ligaments become less tense, allowing progressively greater rotational movement.
Both menisci move slightly anteriorly with full extension at the joint and posteriorly with flexion.
The tight attachment of the inner meniscus to the capsule leads to its lower mobility as compared to the outer one, which is probably related to the higher frequency of damage to the inner meniscus. Retraction of the menisci posteriorly, in which the contraction of the popliteal muscle from the outside and the semimembranous muscle from the inside play an essential role, also serves to prevent their infringement during movements in the knee joint.
The inner and outer condyles of the femur have different configurations. The outer condyle is wider in the anteroposterior and transverse planes, and the inner condyle stands below the outer one in the distal direction. This distal protrusion helps to compensate for the tilt of the mechanical axis in the vertical position so that the transverse axis approaches the horizontal line. The articular surface of the internal condyle is extended anteriorly and as it approaches full extension in the knee joint, the femur rotates inwardly until the remainder of the articular surface of the internal condyle is in contact. The posterior portion of the lateral condyle rotates anteriorly and outwardly, creating a "twisting" moment and stabilizing the knee joint in a fully extended position. When flexion begins, the "unrolling" of the joint is performed by external rotation of the thigh relative to the tibia. The rotational movement responsible for the "twisting" and "untwisting" of the knee joint is carried out around an axis located near the inner condyle of the femur, and it is strongly influenced by the posterior cruciate ligament.
Normally, extension and flexion are possible in the range from 180 to 40 °, but often in some individuals there is an overextension of the knee joint by 5-10 °. When flexing the knee joint to 90 °, the passive rotation of the lower leg in relation to the femur is about 25-30 ° with individual variations. The degree of possible rotation inward is always greater than outward. Sagittal displacement of the lower leg and relative to the femur when bent at the knee joint is possible both anteriorly and posteriorly, but normally by no more than 3-5 mm. When the knee is extended, movements such as adduction and abduction are possible, usually no more than 6-8 °, with a more bent knee position, they should not exceed 15 °.
Surgical approaches to the knee joint
The main vascular and nerve trunks run along the posterior surface of the knee joint, so they are not affected during anterior surgical approaches to the knee joint, metaepiphyseal sections of the femur and tibia.
The anterior approach is used for revision of the knee joint, subtotal synovectomy, open reduction of fractures and osteosynthesis, and total arthroplasty.
The skin and subcutaneous tissue are dissected with a longitudinal incision starting 4-6 cm above the upper pole of the patella, passing over the middle of the patella and continuing distally over the patellar ligament and then along the inner edge of the tibial tuberosity. Then, the tendon of the quadriceps muscle is dissected without damaging the muscle fibers of the vastus internal muscle of the thigh, the capsule of the knee joint, 5 mm inward from the patella and distally to the inner edge of the tuberosity. After that, the synovium is opened. If necessary, the access can be expanded by osteotomy of the tibial tuberosity.

A type of direct approach is the internal parapatellar approach, in which the skin is dissected along the inner edge of the patella, patellar ligament, and tibial tuberosity.
Anteroposterior access - for manipulations on the outer part of the joint, the outer condyle of the tibia, is a mirror image of the anteroposterior access.
For open resection of menisci, transverse or slightly oblique internal or external approaches are used, starting from the corresponding epicondyle of the femur to the patellar ligament.
External access - used for open reduction and osteosynthesis in fractures of the femoral condyles. The incision is made over the lateral surface of the outer condyle of the femur, anterior to the iliotibial tract, and continues distally to the Gerdy tubercle. In parallel to the skin incision, a wide fascia is opened, anterior to the iliotibial tract. Vastus lateralis is separated from the external intermuscular septum, perforating vessels are ligated and the distal part of the femur is exposed. After cutting the outer capsule, the knee joint can be examined.
The posterior-external approach is used for reconstructive operations on the posterior-external parts of the knee joint capsule, for revision of the common peroneal nerve, and for posterior capsulotomy of the knee joint. The incision runs along the posterior edge of the biceps femoris tendon to the posterior edge of the fibular head. With this approach, the common peroneal nerve should always be visualized, exposed proximally and distally, and held onto a holder to prevent its damage. Next, the collateral peroneal ligament and the outer head of the gastrocnemius muscle are exposed. Examination of the femoral-tibial joint can be performed using tibial variation at 90 ° flexion.
The posterior-internal approach is convenient for approaching the vessels of the popliteal fossa and is used for their revision in case of vascular injuries in combination with dislocations of the knee joint; with some modifications, it is also used for the reconstruction of the posterior-internal parts of the capsule and the tibial collateral ligament, as well as for suturing the internal meniscus. The incision runs along the posterior edge of the inner surface of the thigh, above the adductor canal, and continues distally along the posterior-inner surface of the lower leg. Vena saphena and n. safenus needs to be identified and saved. The tendons of the crow's feet are crossed, 2 cm away from their attachment to the tibia. The proximal portion of the pes anserinus is retracted posteriorly with the posterior flap, and the distal portion anteriorly, which allows the inner head of the gastrocnemius muscle to open. Detachment of the latter from the inner condyle of the femur with the limb bent at the knee joint allows access to the popliteal artery from its beginning to trifurcation.
The posterior approach provides an approach to the popliteal fossa masses, the posterior capsule of the knee joint, the posterior parts of the femoral condyles and tibia. The skin incision is usually S-shaped, begins along the posterior-inner edge, over the tendons of the semitendinosus and semimembranosus muscles, bends transversely at the level of the joint space and continues laterally over the head of the fibula. Sometimes a longitudinal midline incision is used. The heads of the gastrocnemius muscle are identified, between which the fascia vena saphena parva and n are pierced. suralis. The popliteal nerve, vein and artery are isolated, and their articular branches are tied if necessary. Then, having retracted the neurovascular bundle, you can approach the posterior parts of the knee joint. The popliteal muscle can be retracted downward and outward.
Examination of a patient with a knee joint lesion
Examination of a patient with pain and dysfunction of the knee joint includes a thorough history taking, physical examination, examination of the limb in general and the joint in particular, X-ray examination, MRI, biomechanical examination, arthroscopy.
Clinical examination
When clarifying the patient's complaints, it is necessary to establish the localization, nature, severity and dynamics of pain in the knee joint, the presence of edema, instability, limitation of movements in it. Clarify the degree of physical activity, the peculiarities of work, everyday life and sports activities, the need for additional support or an external joint fixator.
Studying the anamnesis of the disease, the emphasis is on the presence of single injuries or repeated traumatization of the joint, conservative or surgical treatment and its effectiveness, concomitant diseases.
An objective examination of the knee joint is performed in a patient standing and lying on his back. In a standing position, the axis of the limb, the presence of varus or hallux valgus, flexion contracture of the knee joint, the shape of the joint, the location of the patella, the severity of the relief of the muscles of the thigh and lower leg, the presence of muscle wasting are visually assessed. They reveal lameness when walking, the possibility of full and incomplete squatting, the patient is also asked to reproduce movements that provoke the onset or intensification of pain.
Examination of the patient in the supine position begins with an assessment of the axis of the limb, the shape of the knee joint, hip and lower leg. The axis of the leg is determined based on the fact that the normal line connecting the anterior superior iliac spine, the inner edge of the patella and the big toe is straight.
Next, a palpation examination of the joint is carried out to localize the place of maximum pain, determine the widespread or focal compaction of the synovial membrane, the presence of free fluid in the joint cavity.
Palpating the patella, determine the degree of its displacement inward and outward, soreness, ballooning, increased pain when it is compressed to the condyles of the femur, check the symptom Work - the appearance or a sharp increase in pain under the patella pressed against the femoral sulcus with contraction of the quadriceps femoris muscle.
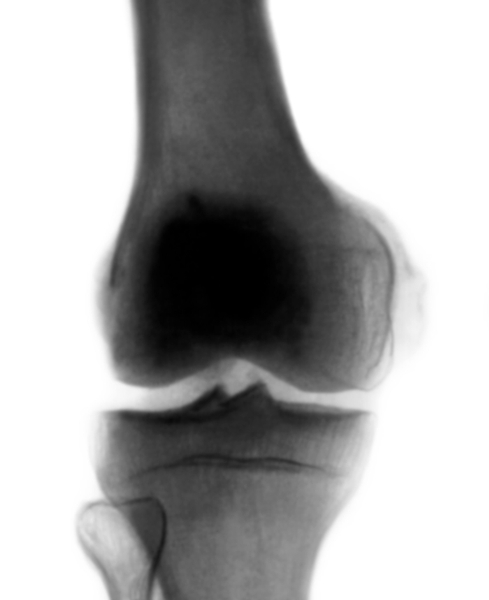
According to radiographs in direct projection, the femoral-tibial angle is determined, formed by the intersection of a line drawn through the middle of the femur diaphysis and the center of its intercondylar fossa, with a line drawn through the middle of the tibial diaphysis and the center of the intercondylar eminence.
X-rays of the knee joint in axial projection in the presence of deforming arthrosis are performed in the patient's prone position, the limb is maximally bent at the knee joint, the foot is grasped with a bandage, with which the patient holds the joint in the flexion position. The cassette is placed under the patella, X-rays are directed perpendicular to it. If the patient cannot bend the leg enough, then the cassette is placed at an angle to the table and the bundle of central rays is tilted accordingly.
The radiographs obtained in this way are used to judge the stage of the degenerative process and the anatomical relationships in the femoropatellar joint.
In young patients, in the absence of degenerative-dystrophic changes in the joint and its dysfunction, axial radiographs are recommended to be performed according to the following technique: the patient is in a sitting position, a specially made splint is placed under the knee joint, controlling the required angle of flexion in the knee joint with a protractor; The patient holds the cassette with the film vertically, pressing it to the thigh 10 cm above the patella, and the X-ray beam is directed perpendicular to the cassette from the shin side. The early signs of lesion of the femoropatellar articulation are better detected if axial radiography is performed with flexion up to 160 °.
On axial radiographs, the presence of the initial signs of arthrosis of the femoropatellar joint, the condition of the bone structures, the form of dysplasia of the patella and femoral-patellar joint are determined. To diagnose early signs of functional disorders on axial radiographs with slight flexion, it is advisable to determine the following indicators:
patellar-femoral index - the ratio of the largest medial and lateral distances between the articular surface of the patella and the femoral groove, on average equal to 1.6;
patellar-femoral angle - the intersection of the lateral facet of the patella with the transverse line connecting the femoral condyles, normally open laterally;
the angle of the femoral groove equal to 137 ° ± 6 °;
the angle of congruence is the intersection of the bisector of the angle of the femoral sulcus and the line connecting the lowest point of the femoral sulcus with the medial edge of the patella, equal to 6 °.
In addition to standard radiographs of the affected knee joint, various functional images are taken to identify the condition of the articular and periarticular structures.
An X-ray from the lower third of the thigh to the middle third of the leg in frontal projection in the standing position of the patient makes it possible to judge the degree of angular deformity by changing the angle between the longitudinal axis of the femur and tibia.
To objectify the study and the possibility of assessing the degree of damage to the ligamentous structures, there is a method of X-ray functional diagnostics. The method consists in carrying out radiography under conditions of loading of the investigated ligamentous structure, when the degree of its insufficiency is indirectly estimated by the degree of displacement of the bones of the knee joint. The load on the ligaments was initially carried out directly by the hands of the researcher, then various devices and devices were developed and implemented for this.
To clarify the state of the intra-articular structures, arthrography of the knee joint is used. The study consists in the intra-articular administration of positive liquid radiopaque drugs that cover the synovial membrane of the cruciate ligaments, menisci, articular cartilage, which allows them to be visually assessed on an X-ray. Arthrography can be performed with single or double contrast. With a single one, 10-15 ml of a liquid contrast agent is used for injection into the joint, and with a double one, 5 ml of a contrast agent is injected together with 4 formations, consisting of 2 or 3 separate bundles of fibers passing from the medial condyle of the femur to the anterior part of the tibial plateau.
In acute injury, the anterior cruciate ligament is presented in the form of loose thin fibers; a hematoma is often found in the area of attachment of the ligament or its rupture. In case of chronic damage, the ligament is completely absent or its image takes the form of unformed dark masses lying in the projection of the ligament.
The posterior cruciate ligament has a clearer structural appearance than the anterior one - a shorter and more intense bundle and can be traced in 2-3 projections. A rupture of the posterior cruciate ligament is manifested by a violation of the regularity of the fibers of the ligament, the expansion of its shadow and an increase in the signal.
The tibial collateral ligament is represented by dark, thin beams of low intensity, extending from the medial condyle of the femur to the proximal medial metaepiphysis of the tibia. On the lateral surface of the knee joint, 4 structures are normally distinguished:
peroneal collateral ligament;
biceps tendon;
hamstring tendon;
iliotibial tract.
All medial and lateral supportive ligaments should be homogeneously dark and have clear, straight contours when the knee is extended. Any expansion of the contours, violation of their length, displacement, increase in signal intensity, as well as the tortuosity of the edges of the structure is regarded as a symptom of damage.
MRI allows, based on changes in signal intensity, to judge the state of bone and cartilage tissue, the synovial membrane of the joint. This contributes to the correct diagnosis of the existing knee joint lesion and the choice of an adequate method of its treatment.
Arthroscopic examination
The development and widespread dissemination of arthroscopy abroad and in our country has brought to a qualitatively new level the possibility of diagnosing and treating pathological conditions of the knee joint, especially at the initial stages in the absence of clear clinical and radiological data allowing to establish the correct diagnosis. Visually and by palpation, arthroscopy allows you to assess the state of the intra-articular structures - cartilage, synovial membrane, menisci and ligaments, choose an adequate method of treatment, perform various interventions under the control of an arthroscope or, if necessary, perform arthrotomy.
The introduction of the arthroscope and instruments for diagnostic arthroscopy is carried out from the anterior inferior approaches:
inferior medial, located in a triangle bounded by the medial edge of the patellar ligament, medial condyles of the femur and tibia;
inferolateral, limited by the lateral edge of the patellar ligament and the lateral condyles of the femur and tibia.
If necessary, use additional accesses.
Having outlined the accesses in the 90 ° flexion position in the knee joint, two incisions are made in the skin and a fibrous capsule 5 mm long, a trocar with a blunt obturator is perforated in the synovial membrane, directing it to the intercondylar fossa of the femur, the limb is extended at the knee joint, the trocar is inserted into the upper volvulus ... The obturator is replaced with an arthroscope, a fluid or gas supply system is connected to the joint. It should be noted that performing arthroscopy in a gas environment requires a special device - an insufflator, which has electronic monitoring of intra-articular pressure.
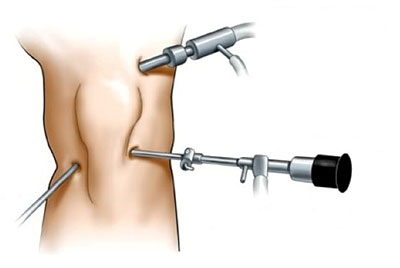
The study of the knee joint begins with the upper fold. The condition of the synovium, scars and adhesions, and the presence of intra-articular bodies are visually assessed.
Then the arthroscope is moved to the femoral-patellar joint. Examine the articular cartilage of the patella and femoral sulcus, the shape of their articular surface, determine the lateral and longitudinal mobility of the patella in the femoropatellar joint. For this, the arthroscope is placed at the lower pole of the patella, bending and unbending the limb in the joint, observing the symmetry of the joint space under the inner and outer facets, the uniformity of the entry of the patella into the groove.
The examination of the superior volvulus and the femoropatellar joint is completed by examining the mediopatellar synovial fold, establishing its anatomical features, revealing local pathological changes.
Under visual control, the arthroscope is moved over the medial condyle of the femur to the inner part of the femoral-tibial joint, keeping the edge of the condyle of the femur and the medial part of the capsule in sight, the limb is bent at the knee joint by 30-60 ° and retracted to carefully examine the internal meniscus. synovium and articular surfaces of the femur and tibia. For a more detailed study of these structures, flexion, extension and rotational movements of the lower leg, percutaneous palpation in the projection of the joint with the fingers of the free hand are performed.
On examination, attention is paid to the shape of the meniscus, the possibility of its displacement, color, shine, tissue density, surface structure, vascular changes in the region of the horns and the base of the meniscus. Having found damage to the meniscus, determine its type, localization and length. Clarify the presence and nature of damage to the articular cartilage of the femur and tibia.
From the medial section, the arthroscope is moved to the intercondylar region, where, first of all, the anterior cruciate ligament is examined along its entire length. Then the size, structure, presence of inflammatory or cicatricial changes in the fatty body are assessed. The hypertrophied fatty body is examined during flexion and extension in the joint to identify possible infringement of its lobules between the articular surfaces.
Arthroscopy is completed by examining the outer part of the joint. Evaluation of the state of the lateral meniscus, articular surfaces of the femur and tibia and the synovial membrane is carried out by bringing the lower leg bent at an angle of 95-100 °.
If the intervention is limited to diagnostic arthroscopy, then the joint is washed with 1.5-2 liters of isotonic sodium chloride solution, sutures are applied to the skin incisions. According to the indications, manipulations on the articular structures are performed under the control of an arthroscope.